Safe Transportation to and from Quarantine and Isolation Spaces
April 14, 2020This guide would be appropriate for Continuums of Care, Coordinated Access Networks, and Balance of States designing how to properly transport clients to and from medical facilities.
The relevant sources have been listed in each section, and notes from Built for Zero’s internal quality control check can be found at the end of the document. It is further advised that beyond this guidance that you coordinate with public health partners in designing an approach.
Given that the clinical picture of COVID-19 is ever changing, and that the information about response is changing in turn, Built for Zero anticipates there might be new information on this topic. Please keep an eye out for updated information.
When is transportation needed for individuals experiencing homelessness?
Transportation should be utilized when:
- Alternate care sites are not appropriate and medical care at a health care facility is necessary. This is determined by the level of care the individual requires, which includes:
- General (non-acute) care: where the individual requires low-level care for mildly to moderately symptomatic COVID-19 patients. In this level, patients may need oxygen, do not require extensive nursing care, and can generally move about on their own.
- Acute care: where the individual requires critical care and advanced cardiovascular life support
- An individual has been discharged from medical care and needs to be housed in a non-congregate setting.
- An individual has tested positive for COVID-19 or is suspected positive (classified as a person under investigation) and needs transportation to a quarantine and isolation setting or a permanent housing situation from congregate living or unsheltered homelessness.
Sources
- CDC: Responding to Coronavirus disease 2019 (COVID-19) among People Experiencing Unsheltered Homelessness
- CDC: Infection Prevention and Control Considerations for Alternate Care Sites
- Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings
- CDC: Discontinuation of Transmission-Based Precautions and Disposition of Patients with COVID-19 in Healthcare Settings (Interim Guidance)
What modes of transportation are appropriate?
- Transporting an individual experiencing homelessness will require the use of individual transportation methods, such as:
- Medical transport, if available
- Agency vans
- Taxis
- Retrofitted and repurposed public transportation vehicles designated solely for the transportation of people with COVID-19 or symptomatic individuals
- Other individual transportation modes like Uber, Lyft
- Please see below for safety considerations related to passenger personal protective equipment (PPE) and guidance on preparing and cleaning the vehicles like agency vans, taxis and other individual modes like Uber or Lyft.
Sources
- HUD: Strategies for Improving Homeless People’s Access to Mainstream benefits and Services
- County of Santa Clara & City of San Jose: Addressing COVID-19 in the Homeless Community
- University of California San Francisco Curry International Tuberculosis Center: Preventing Aerosol Transmissible Disease: A Reference Guide for Homeless Shelters and Residential Treatment Facilities
- VA: Disaster Preparedness to Promote Community Resilience
- American Public Transportation Association: Summary: A Guide for Public Transportation Pandemic Planning and Response (NCHRP Report 769)
- USICH: COVID-19 Planning and Response: Isolation and Quarantine: Lessons Learned from Seattle & King County
- CDC: Interim Guidance for Emergency Medical Services (EMS) Systems and 911 Public Safety Answering Points (PSAPs) for COVID-19 in the United States
What processes and barriers should be used in the vehicle?
- Processes for transporting individuals should include:
- Maintaining a list of all vehicles with proper documentation
- Determining how the vehicles will be deployed
- Equipping vehicles with emergency radios or phones so that staff have the ability to communicate, go-kits, and emergency supplies
- Space:
- Few enough passengers are transported to ensure there is proper distance between them, with 6 feet as the ideal distance and 3 feet as the minimum
- Staffing:
- A staff member must accompany to ensure safety for the client, whether transporting an individual experiencing homelessness in an agency vehicle or another individual transportation method to a medical care facility or from a medical care facility to a non-congregate setting
- Vehicle:
- In order to prevent the spread of disease while transporting, an agency utilizing their vehicle for transport should:
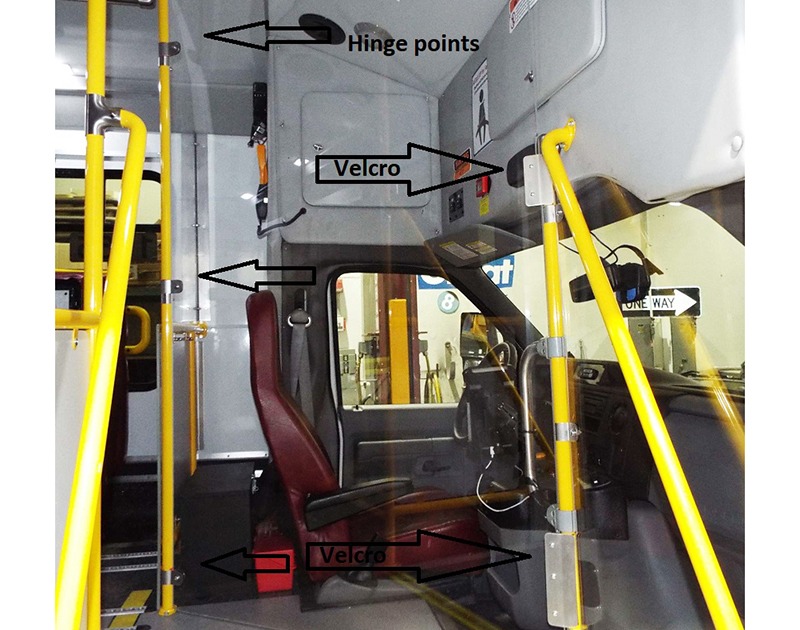
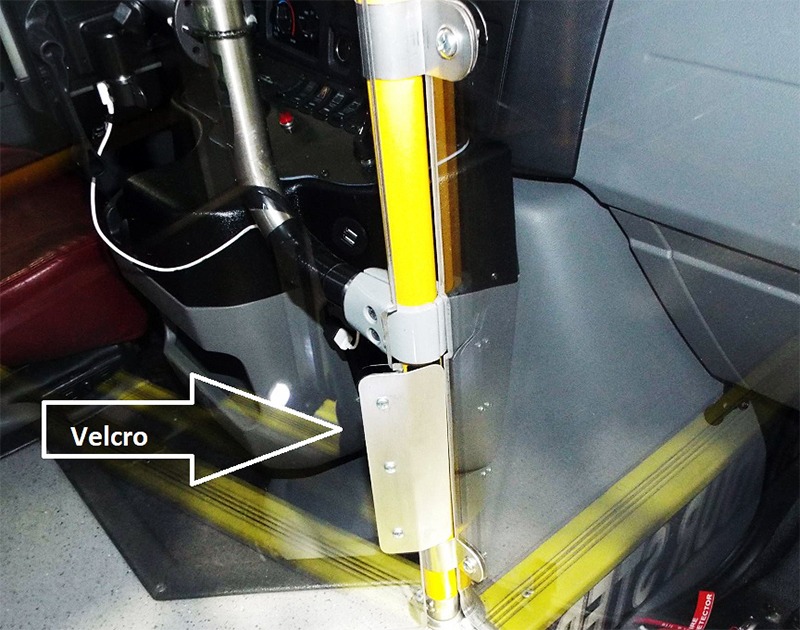
- Ensure that the driver and the passengers are separated by some barrier, such as plexiglass, if feasible
- That vehicle is equipped with and driver wears PPE
- The vehicle is cleaned routinely to minimize surface contamination
- That heating, ventilation, and/or air conditioning is controlled to reduce the spread of contamination. Learn more in: How should clients with exposure history and symptoms be transported to a health care facility?
- In order to prevent the spread of disease while transporting, an agency utilizing their vehicle for transport should:
Sources
- HUD: Strategies for Improving Homeless People’s Access to Mainstream benefits and Services
- County of Santa Clara & City of San Jose: Addressing COVID-19 in the Homeless Community
- University of California San Francisco Curry International Tuberculosis Center: Preventing Aerosol Transmissible Disease: A Reference Guide for Homeless Shelters and Residential Treatment Facilities
- VA: Disaster Preparedness to Promote Community Resilience
- American Public Transportation Association: Summary: A Guide for Public Transportation Pandemic Planning and Response (NCHRP Report 769)
- COVID-19 Planning and Response: Isolation and Quarantine: Lessons Learned from Seattle & King County
- CDC: Interim Guidance for Emergency Medical Services (EMS) Systems and 911 Public Safety Answering Points (PSAPs) for COVID-19 in the United States
What entities should you partner with when providing transportation?
Coordination across several sectors is required to ensure the health and protection of individuals experiencing homelessness while they’re transported during this time. Logistic plans need to be clearly communicated across sectors. The following partners should be involved:
- Hospitals and healthcare facilities to ensure:
- Planning and logistics for safely transporting COVID-19 patients and persons under investigation (PUI) to their facilities
- Planning for safely discharging COVID-19 patients to a designated location where they can continue to get care.
- Behavioral health teams should be involved in planning and present to facilitate continued access to support for people with behavioral health issues.
- Public Transit Authority, to utilize or repurpose paratransit or other vehicles not in use due to the pandemic for the safe transport of COVID-19 patients.
- Upon discharge from a medical care facility, an identified respite care or other isolation site location for the individual should be made in coordination with the health department or other appropriate entity.
Example
Seattle-King County, Washington’s Transportation for Pandemic Response provides critical mobility when emergency response resources are strained.
- Transportation for Pandemic Response (TPR) is supplemental transportation service for people who are confirmed to have COVID-19; those that are symptomatic, but have not received a confirmed diagnosis for the illness from isolation and quarantine sites; and for discharge of COVID-19 patients to isolation and quarantine sites.
- Partnerships
- TPR is a partnership with King County’s Department of Community and Human Services, Seattle-King County Department of Public Health, King County Metro, and MV Transportation, the paratransit contractor for the county. Seattle-King County brought together the following to build out this program:
- Legal
- Health Department
- Public Transit
- Component Supply Center
- Safety
- Labor Liaison
- Dispatch
- Sanitation
- Drivers and other operations
- Vehicle Maintenance
- TPR is a partnership with King County’s Department of Community and Human Services, Seattle-King County Department of Public Health, King County Metro, and MV Transportation, the paratransit contractor for the county. Seattle-King County brought together the following to build out this program:
- Scope
- The partnership agreed to engage its Access paratransit contractor, MV Transportation, to create a service to move COVID-19 positive or symptomatic individuals to and from: public health isolation or quarantine sites, medical facilities, homeless shelters, assisted living facilities, and other locations housing vulnerable individuals, including personal homes.
- Installing Physical Shields
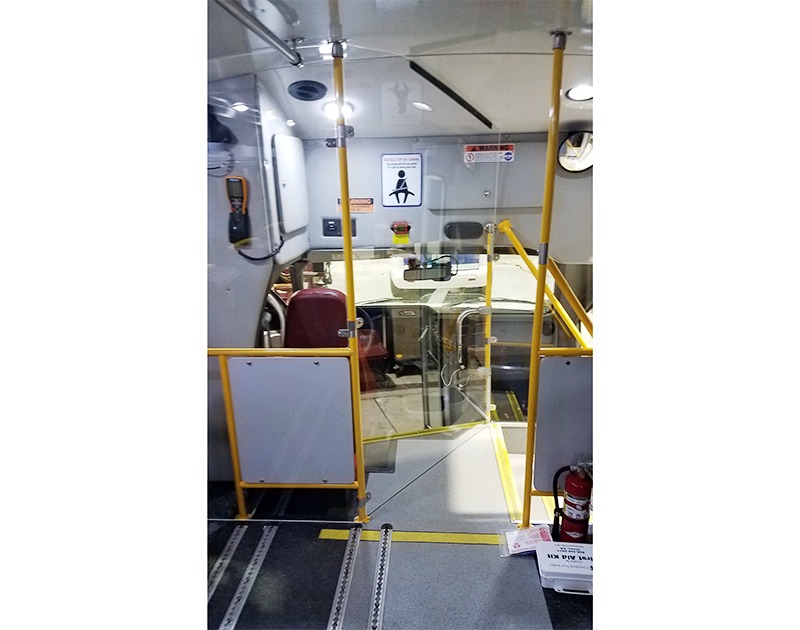
- At MV’s request, Metro’s Component Supply Center shop is custom outfitting a small fleet of Access vehicles with custom floor-to-ceiling driver compartment shields to protect drivers.
Transportation for Pandemic Response from Seattle-King County



Sources
- CDC: Responding to Coronavirus disease 2019 (COVID – 19) among People Experiencing Unsheltered Homelessness
- Email from King County Government: Recognition of a successful launch of Transportation for Pandemic Response (TPR)-King County, WA
What type of personal protective equipment (PPE) needs to be utilized by staff transporting individuals?
Both clients and passengers should have proper PPE.
- Face masks are one alternative until the supply chain is restored, according to the CDC. Respirators should be prioritized for healthcare professionals engaging in procedures that are likely to generate respiratory aerosols, which would pose the highest exposure risk.
- Eye protection, gown, and gloves continue to be recommended.
- If there are shortages of gowns, they should be prioritized for:
- Healthcare professionals performing aerosol-generating procedures
- Care activities where splashes and sprays are anticipated
- High-contact, patient-care activities that provide opportunities for transfer of pathogens to the hands and clothing
- If there are shortages of gowns, they should be prioritized for:
Cloth Face Coverings
- The CDC recommends that all people wear cloth face coverings in public settings where other social distancing measures are difficult to maintain, especially in areas of significant community-based transmission.
- However, homemade masks are not considered PPE, since their capability to protect health care providers is unknown. Caution should be exercised when considering this option.
- Homemade masks should ideally be used in combination with a face shield. Face shields provide full face coverage: they should cover the entire face, including mouth, nose, and eyes. They should cover the forehead, extend below the chin. and wrap around the side of the face. The extended faceshield guidance is informed by the fact that it may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes. This is not thought to be the main way the virus spreads, but the CDC and others are still learning more about this virus.
Emergency Medical Services (EMS) Clinicians:
- EMS clinicians who will directly care for a patient with a possible COVID-19 infection or who will be in the compartment with the patient should follow standard precautions and use the PPE as described below. Recommended PPE includes:
- N95 or higher-level respirator or face mask (if a respirator is not available)
- N95 respirators or respirators that offer a higher level of protection should be used instead of a facemask when performing or present for an aerosol-generating procedure. Aerosol generating procedures as defined as those that, when performed on a patient with known or suspected COVID-19 could generate infectious aerosols. In particular, procedures that are likely to induce coughing (e.g., sputum induction, open suctioning of airways) should be performed cautiously and avoided if possible.
- When the supply chain is restored, fit-tested EMS clinicians should return to use of respirators for patients with known or suspected COVID-19 infection.
- Eye protection (i.e., goggles or disposable face shield that fully covers the front and sides of the face). Personal eyeglasses and contact lenses are NOT considered adequate eye protection.
- A single pair of disposable patient examination gloves. Change gloves if they become torn or heavily contaminated.
Gowns. If there are shortages of gowns, they should be prioritized for aerosol-generating procedures, care activities where splashes and sprays are anticipated, and high-contact patient care activities that provide opportunities for transfer of pathogens to the hands and clothing of EMS clinicians (e.g., moving patient onto a stretcher).
- N95 or higher-level respirator or face mask (if a respirator is not available)
Drivers that provide direct patient care:
- These drivers should wear all recommended PPE. A respirator or face mask should continue to be used during transport.
- Removing PPE. On arrival, after the patient is released to the facility, EMS clinicians should remove and discard PPE and perform hand hygiene. Used PPE should be discarded in accordance with routine procedures.
All personnel should avoid touching their face while working.
- Other required aspects of standard precautions (e.g., injection safety, hand hygiene) can be found in the Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings.
Source
The guidance from the Centers for Disease Control and Prevention applies to all first responders, including law enforcement, fire services, emergency medical services, and emergency management officials, who anticipate close contact with persons with confirmed or possible COVID-19 infection in the course of their work. We have applied it here, as staff working in the homelessness response system with people with COVID-19 or persons under investigation (PUI) will likely be in close contact with such persons.
- Toronto Public Health: Infection Prevention and Control Guide for Homelessness Service Settings
- CDC: Interim Guidance for Emergency Medical Services (EMS) Systems and 911 Public Safety Answering Points (PSAPs) for COVID-19 in the United States
- CDC: Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings
- CDC: Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission
How should clients with exposure history and symptoms be transported to a health care facility?
If a client with an exposure history and signs and symptoms suggestive of COVID-19 requires transport to a health care facility for further evaluation and management, the following actions should occur during transport:
- Notify the receiving health care facility that your client has an exposure history and signs and symptoms suggestive of COVID-19, so that appropriate infection control precautions may be taken prior to client arrival.
- Keep the client separated from other people as much as possible.
- Family members and other contacts of patients with possible COVID-19 infection should not ride in the transport vehicle, if possible. If riding in the transport vehicle, they should wear a face mask.
- Isolate the ambulance driver from the patient compartment and keep pass-through doors and windows tightly shut.
Vehicles that have isolated driver and patient compartments (ideal):
- Close the door/window between these compartments before bringing the patient on board.
- Vehicle ventilation in both compartments should be in non-recirculated mode to maximize air changes that reduce potentially infectious particles in the vehicle.
- If the vehicle has a rear exhaust fan, use it to draw air away from the vehicle, toward the patient-care area, and out the back end of the vehicle.
- If the vehicle is equipped with a supplemental recirculating ventilation unit that passes air through High Efficiency Particulate Air (HEPA) filters before returning it to the vehicle, use it to increase the number of air changes per hour (ACH).
Vehicle without an isolated driver compartment and ventilation:
- Open the outside air vents in the driver area and turn on the rear exhaust ventilation fans to the highest setting. This will create a negative pressure gradient in the patient area.
Source
How should staff clean a vehicle used to transfer a person infected with or suspected of having COVID-19?
Emergency Medical Services (EMS) transport vehicles
- NOTE: As much of this guidance should be followed as possible and appropriate when using vehicles that are not EMS transport vehicles:
- After transporting the patient, leave the rear doors of the transport vehicle open to allow for sufficient air changes to remove potentially infectious particles.
- The time to complete transfer of the patient to the receiving facility and complete all documentation should provide sufficient air changes.
- When cleaning the vehicle, EMS clinicians should wear a disposable gown and gloves. A face shield or face mask and goggles should also be worn if splashes or sprays during cleaning are anticipated.
- Follow environmental cleaning and disinfection procedures, including the provision of adequate ventilation when chemicals are in use. Doors should remain open when cleaning the vehicle.
- Routine cleaning and disinfection procedures (e.g., using cleaners and water to pre-clean surfaces prior to applying an EPA-registered, hospital-grade disinfectant to frequently touched surfaces or objects for appropriate contact times as indicated on the product’s label) are appropriate for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, the virus that causes COVID-19.) in health care settings, including those patient-care areas in which aerosol-generating procedures are performed.
- Products with EPA-approved emerging viral pathogens claims are recommended for use against SARS-CoV-2, the virus that causes COVID-19.
- Clean and disinfect the vehicle in accordance with standard operating procedures. All surfaces that may have come in contact with the patient or materials contaminated during patient care (e.g., stretcher, rails, control panels, floors, walls, work surfaces) should be thoroughly cleaned and disinfected using an EPA-registered hospital-grade disinfectant in accordance with the product label.
- Clean and disinfect reusable patient-care equipment before use on another patient, according to manufacturer’s instructions.
- Dispose of used PPE and regulated medical waste by following standard operating procedures.
- Contain and launder used linen following standard operating procedures. Avoid shaking the linen. Read more here
Non-EMS-transport vehicles:
- All drivers who are transporting people infected with COVID-19 or suspected of infection (PUI) should follow the above guidance related to appropriate PPE and preparing the interior of non-EMS-transport vehicles.
- Minimize the number of vehicles shared by employees to limit the spread of the virus between different users of the same vehicles where possible.
- Drivers who are feeling sick should be instructed to stay home.
- Drivers should be trained to execute on the following guidance:
- Wash hands regularly and whenever soiled with plain soap and warm water for at least 20 seconds. When drying hands, disposable paper towels are preferred.
- If soap and water are not available, an alcohol-based hand sanitizer (ABHS) can be used as a temporary measure until hand washing can be done. ABHS containing 60-90% alcohol concentration (optimally over 70%) are the most rapidly active of all agents used in hand disinfection. However, ABHS may not be effective when there is organic material on your hands (e.g. after using the toilet). For this reason, ABHS alone should not be used on visibly soiled hands. Use wipes to remove soil, followed by ABHS.
- Avoid touching eyes, nose and mouth with unwashed hands.
- When coughing or sneezing, drivers should:
- cough or sneeze into a tissue or the bend in the arm, not into hands.
- dispose of any tissues that have been used as soon as possible in a lined wastebasket.
- wash/sanitize hands for 20 seconds afterwards.
Cleaning and disinfecting before trips:
- Make sure vehicle interiors are clean and hygienic by wiping surfaces with disinfectant.
- Products with EPA-approved emerging viral pathogens claims are recommended for use against SARS-CoV-2, the virus that causes COVID-19.
- High-touch surfaces in trucks that should be regularly cleaned include, but are not limited to:
- Keys or FOBs
- Starter button on vehicles with FOBs
- Inside and outside door handles; Inside door grab handles, pads and armrests
- Steering wheel
- Shift lever and console
- Dashboard
- Power window and power door lock switches
- Radio and climate control buttons
- Turn signal and wiper stalks
- Seat and seat adjuster
- Touch screen
- Any other parts that are commonly used and that may have been touched (glove compartment, hood, trunk, van panel door handles, pick-up tailgate handle, sleeping areas, for example).
- Dispose of soiled cleaning clothes, disinfection cloths, disposable gloves, and any other items in contact with respiratory tract secretions in a waste disposal bag.
- Wash hands when finished using proper hand-washing techniques.
Cleaning and disinfecting after trips:
- Repeat a thorough cleaning of high-touch surfaces with appropriate disinfectants as described above.
Sources
- CDC: Interim Guidance for Emergency Medical Services (EMS) Systems and 911 Public Safety Answering Points (PSAPs) for COVID-19 in the United States
- EPA: List N: Disinfectants for Use Against SARS-CoV-2
- Public Health Agency of Canada: Federal safety guidance to protect drivers and limit the spread of COVID-19 in commercial vehicle operations
When is transportation not necessary?
General care and non-emergency situations:
- Hospitalization, and therefore transportation to a medical facility, is not necessary if an individual has been determined by a health care professional to need general care.
- General care patients can be be monitored and cared for through a variety of means such as:
- A health care professional, if a partnership with a hospital or clinic has been established
- Properly trained staff who are in coordination with a health care professional to assist the individual with following care instructions
- Use of telehealth, wherein patients are seen virtually by a healthcare professional to address health concerns
Examples of general care:
- Wake County, North Carolina, social service providers working with people experiencing homelessness have been provided with tablets and 1,200 telehealth visits through a Durham-based telemedicine company so that those with that are general care patients can be cared for without utilizing an emergency room or a hospital.
- Austin and Travis County, Texas, are utilizing telehealth to provide mental health treatment and making face-to-face visits by appointment only as needed.
Sources
- HUD & CDC: Non-Congregate Approaches to Sheltering for COVID – 19 Homeless Response
- CDC: Responding to Coronavirus disease 2019 (COVID – 19) among People Experiencing Unsheltered Homelessness
- Raleigh News & Observer: Here’s how the homeless are being screened in Wake
- Austin American-Statesman: City chooses hotels as isolation sites to house homeless coronavirus patients
What COVID-19-specific funding sources or other funding sources can be used to cover the expenses associated with transporting individuals?
Private
- Utilization of medical respite care programs, which deliver health care and support services to individuals who need ongoing care but do not require hospitalization.
- Medical respite care is short-term residential care that allows individuals experiencing homelessness the opportunity to rest in a safe environment while accessing medical care and other supportive services. This care can be for acute and post-acute care for persons who are not ill enough to be in a hospital and can be offered in a variety of settings.
- These are usually funded by hospitals and private donations as a combination.
- These are setup through contracts or memoranda of understanding (MOUs).
- See National Healthcare for the Homeless Council for more information on how to set up a medical respite care program.
- Local funders and philanthropic organizations may grant opportunities available to cover expenses that have arisen due to COVID-19.
- Medical respite care is short-term residential care that allows individuals experiencing homelessness the opportunity to rest in a safe environment while accessing medical care and other supportive services. This care can be for acute and post-acute care for persons who are not ill enough to be in a hospital and can be offered in a variety of settings.
Federal
- Medicaid Waivers. Section 1135 waivers and 1115 Medicaid demonstrations allow for the U.S. Department of Health and Human Services for states to allow for care in alternative settings from a hospital or doctor’s office.
- To determine if your state has applied for a 1135 waiver and 1115 Medicaid demonstration, contact your state’s Medicaid agency.
- FEMA Assistance. Under emergency declaration, FEMA is authorized to reimburse local governments for costs associated with “emergency protective measures” in response to the COVID-19 pandemic. Eligible emergency protective measures taken to respond to COVID-19 at the direction or guidance of public health officials may be reimbursed under Category B of FEMA’s Public Assistance program. These funds will not duplicate assistance provided by other federal agencies. This can cover:
- Non-deferrable medical treatment of infected persons in a shelter or temporary medical facility
- Related medical facility services and supplies
- Movement of supplies and persons
- Emergency medical transport
- Community Development Block Grant (CDBG). CDBG funds have been used to cover ride-share transportation, such as Lyft.
Sources
- National League of Cities: Seeking FEMA Assistance to the COVID-19 Pandemic
- National Health Care for the Homeless Council: Medical Respite Care
QUALITY CHECK
Learn more about our process for vetting information.


